November  2016
2016
Integrate Technology With Process Improvement
By Swami R. Reyes, MCLSS, JD, LSSBB
For The Record
Vol. 28 No. 11 P. 28
Designing effective workflows and robust technology adoption and implementation will have the most impact on improving efficiency, patient experience, and care coordination, according to a new poll of more than 170 health care quality professionals conducted in late August by the American Society of Quality (ASQ).
As per www.usbusinessexecutive.com, "the integration of health information technology into primary care includes a variety of electronic methods that are used to manage information about people's health and health care, for both individual patients and groups of patients. The use of health IT can improve the quality of care, even as it makes health care more cost-effective."
In fact, according to the ASQ survey, the following technologies were found to have the most impact on improving patient experience and care coordination:
• incorporation of wearable sensors, remote patient monitoring, and other caregiver collaboration tools (71%);
• smartphones, tablets, and applications providing a wealth of information for physicians and other clinicians (69%); and
• online communications along every step of the patient process, including registration and payment (69%).
Workflow, Reimbursement Effects
A key to the successful implementation of HIT is to recognize its impact on both clinical and administrative workflows. Once implemented, HIT can provide information to help an organization reorganize and improve workflow. It also can improve the quality of care and cut costs via the development of a secure EHR system capable of making health information available electronically when and where it is needed.
HIT also plays a role in reimbursement. The Medicare Access and CHIP Reauthorization Act (MACRA), which was enacted in 2015 to replace the sustainable growth rate for physician payment, has started to become a factor in hospital and clinical settings. The rule institutes new rules for quality reporting and payment policies that substantially change the status quo for Medicare's physician reimbursement.
MACRA focuses on the two main pathways for physician payments: the Merit-Based Incentive Payment System and alternative payment models.
How these pathways are implemented via technology will have a major impact not only on clinician payment but also on how health care organizations deliver care and the cost of care.
Paper simply won't work in this new reimbursement environment where technology is now more integrated, affordable, and easier to install and maintain. MACRA focuses on the use of technology in several areas, including reporting patient outcomes and achieving interoperability. Current programs such as the physician quality reporting system and meaningful use will still exist in some form as part of MACRA, and there will be an increased push toward accountable care and value-based reimbursement.
While MACRA may be a challenge, it also offers a huge opportunity. For those who are well prepared, the incentives can be significant—a more than 25% increase in Medicare payments. There's also the chance to exceed 100% reimbursement in 2019 based on an organization's 2017 performance.
"It's imperative to remember that technology is an enabler—the focus needs to be less on implementing the system and more on implementing the changes in the business enabled by that system," according to Liam Walsh, a principal at research firm KPMG, in the report "Digital Health: Heaven or Hell."
Hurdles to Clear
Ironically, even successful HIT implementations can sometimes make efficient care delivery more difficult. Recent surveys of US physicians show that EHRs are among the principal causes of professional frustration. According to the ASQ poll, the following hurdles are "very difficult" for health care organizations to overcome as they work to implement technology that will improve quality, efficiency, and reduce cost:
• resistance to change from physicians and staff due to a perceived impact on time/workflow and an unwillingness to learn new skills (70%);
• high costs of implementing IT infrastructure and services, and unproven return on investment (64%); and
• problems with complex new devices, poor interface between multiple technologies, and the haphazard introduction of new devices that could cause patient errors (61%).
"We in health care know that there are always drawbacks to technology. While not a panacea, technology can help engage patients, increase access to care, help improve safety, and make data collection easier," says Susan Peiffer, chair of ASQ's health care division and performance improvement specialist at Hospital Sisters Health System Western Wisconsin Division.
In the new global, ever-evolving health care landscape, digital technologies are becoming increasingly normalized into the everyday delivery of care. This creates both top-down and bottom-up momentum for change. Patient-facing technologies are at the center, reflecting the impact that this new ecosystem of self-monitoring and decision support will have on their experience and quality of care.
Navigating this new landscape—one filled with many pitfalls—is challenging for organizations and their leaders. Cost and expectations of quality mean that doing nothing is no longer a sustainable option.
The intense competitive nature of the industry, the constantly changing rules and regulations, the need for effective navigation of the technology conundrum, the pressure to reduce costs and increase profits, and the drive to provide patient-centered quality outcomes are no match for "status quo" solutions; change is evolving at lightning speed.
Where implementations have failed, technology often has been layered on top of existing structures and work patterns, creating an additional workload for the health care team. The technologies that have generated the greatest immediate benefits have been carefully designed to make jobs and patient interaction easier, and featured considerable investment in both the design of the tool and workflow redesign.
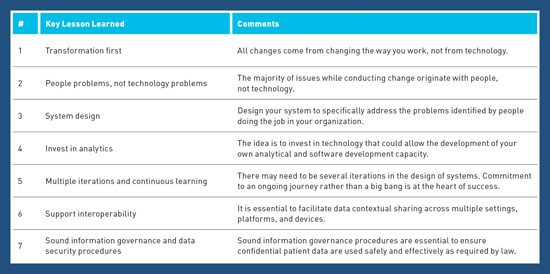
For organizations looking to achieve a successful digital transformation, the KPMG report "Digital Health: Heaven or Hell" has identified the following seven key factors:
What's Next
Technology is rewriting health care relationships. In the next decade, computing will be universal and less visible, time spent by staff on administrative tasks and routine communication will be drastically reduced, new roles and competencies will be added, and organizational and professional boundaries will be far less visible.
In the last 60 years, the world has seen an unprecedented technology transformation in all aspects of life but perhaps no sector has been more affected than health care. The difference today between successful and failed HIT adoption and implementation can be reduced to one simple component: speed of transformation.
— Swami R. Reyes, MCLSS, JD, LSSBB, is an ISO 9000 lead auditor with more than 30 years of global experience in operational excellence, executive leadership, customer satisfaction, and quality and process management. Reyes, who works with corporate, government, health care, and not-for-profit organizations, is chair-elect for the ASQ Healthcare Division and chair of the health care body of knowledge content group.



