December 17, 2012
December 17, 2012
Setting the Stage for MU’s Next Act
By Selena Chavis
For The Record
Vol. 24 No. 23 P. 10
As the third step on the epic journey known as meaningful use begins to take shape, here’s a look at what hospitals can expect.
Healthcare providers currently are knee-deep in meaningful use stage 2 preparations following the release of the final rule this past summer. The race is on to qualify for incentives in a timely fashion, and while the road to get there will be complex for many organizations, industry professionals point to a need to simultaneously consider the coming expectations for stage 3.
Couple these preparations with ICD-10 and other federal performance-based initiatives covered under the Affordable Care Act (ACA) and it’s imperative that hospitals attempt to apply resources to these efforts synergistically.
“Everything is happening at the same time,” says Diana Warner, MS, RHIA, CHPS, FAHIMA, director of HIM solutions at AHIMA. “Aligning with the correct initiative at the correct time to maximize incentive is critical.”
Charlie Jarvis, vice president of health reform for NextGen Healthcare, agrees, adding that the initiatives are designed to work together since the HITECH Act and the ACA share the same authors. “I think they complement each other very nicely,” he says. “Providing that we do the most important thing—reform the delivery system—it will work.”
With the initial comment period well under way for stage 3, industry professionals offer insights on what to expect going forward.
Stage 3 Timetable
As preparations for stage 2 unfold across the healthcare landscape, the Centers for Medicare & Medicaid Services (CMS) has jump-started plans to finalize the stage 3 draft and comment period. While past experience with stages 1 and 2 suggested a much later rollout process, draft recommendations were delivered to the Office of the Federal Register for publication in November to initiate a timetable for request for comments. During the comment period, stakeholders can review various concepts, draft recommendations, and provide feedback.
“There’s so much pressure from the industry for us to provide insight into what they can expect,” explains Charlene Underwood, MBA, FHIMSS, senior director of government and industry affairs for Siemens Healthcare and a member of the Meaningful Use Work Group. “That’s the reason for the early timetable.”
The Office of the National Coordinator for Health Information Technology provided a 45-day comment period so the committee could begin synthesizing the comments at the beginning of 2013. Underwood suggests that ideally the committee could then present revised recommendations in March with the final draft submitted to Health and Human Services in May.
This timetable follows a much more aggressive path than previous expectations, according to Jarvis, who says the patterns with stages 1 and 2 would have suggested an early draft release in mid-2014 with a nine-month window for the comment period and revisions and draft finalization in the summer of 2015.
The early release of the stage 3 draft recommendations and the provision of a brief 45-day comment period have drawn criticism from several professional groups, including the American Medical Association (AMA) and the American Hospital Association (AHA). In the October meeting of the Health IT Policy Committee, the AHA recommended that the committee consider a delay in the request for comments since providers will be attesting to stage 1 and others will have only begun digesting stage 2. The association also suggested that the comment period be extended to 60 days to ensure responses from a larger sample of stakeholders that are thoughtful and based on experience.
In the same meeting, the AMA advocated that the CMS conduct an evaluation process relevant to current initiatives, suggesting that it build in a short questionnaire for providers to determine the feasibility of the measures going forward.
The one caveat to the current timetable unfolding is that the CMS will be watching stage 2, Underwood notes. While actions at the highest government levels indicate the industry is moving in two-year phases, with stage 2 coming online in 2014 and stage 3 in 2016, other factors may necessitate changes. “CMS will monitor what is happening in stage 1 and stage 2, and has final authority for issuing the regulation,” Underwood points out.
Jarvis agrees, noting that “if the past is a predication of the future, we should take it [current timetable] with a grain of salt.” He points out that stage 2 was delayed one year for practical reasons and wouldn’t be surprised if stage 3 rolls out in 2017 or later.
The Details
According to Jarvis, stage 3 essentially will serve as an extension of the overall process of market reform that is currently under way. Many of the requirements under consideration follow the philosophical road map of the first two stages, moving deeper into more meaningful use of EHRs and data sharing.
In fact, according to Brian Levy, MD, senior vice president and chief medical officer for Health Language, there likely will not be any surprises—no new standards and no major changes between stages 2 and 3. The new rules are expected to continue expansion of current initiatives. “There will be more clinical quality measures and a higher percentage of patients to report on,” he notes.
The focus of stage 3 is improved outcomes, with specific emphasis on greater use of clinical decision support, computerized physician order entry, structured data, and patient engagement. Hospitals will need to be able to leverage an EHR to perform tasks such as track individual care goals, review and receive immunization data from public health registries, electronically report adverse events to public health agencies, identify care teams and track roles and responsibilities across care settings, and enable input by care team members, patients, and other providers.
Privacy and Security Considerations
According to Underwood, the need for consistent privacy and security standards will be heightened as the industry moves into stage 3 because there will be more collaboration between systems. Request for comment questions raised about privacy and security include potential issues associated with provider authentication for remote access, HIPAA security risk assessments and the need to account for disclosures, surveillance for unauthorized access, and incident investigation.
“A lot of provisions are in place,” Underwood notes. “The challenge is the broader application of those provisions.”
It also will be a challenge to find the right balance between security and consumer engagement, which is a focal point of meaningful use objectives going forward. Two primary objectives outlined for stage 3 include patient access to self-management tools and access to comprehensive patient data through patient-centered health information exchange.
“We’re trying to move the industry to a more patient-centric view,” Underwood explains. “The challenge is going to be changing the culture.”
Warner points out that patient access is an important privacy right, and parameters outlining these needs should be strengthened more in stage 3. “Consumer engagement is critical to achieve the desired outcomes,” she says. “We need to advocate that privacy and security is not meant to be a barrier. We need to be their advocate for ensuring information is shared in the manner it’s meant to be shared.”
Success will hinge on a patient’s ability to engage in care, Jarvis says. “That’s the fallback of taking too strict a focus on privacy,” he notes. “We need to engage a practical approach and not be so strict we work against ourselves.”
Impact to HIM
Levy suggests that stage 3 will have a favorable impact on HIM professionals because they “will have access to more information and be able to make better decisions.”
In the past, he points out there’s been a divide between what goes on “upstairs” in the clinical world and what goes on “downstairs” in the HIM and billing departments. As meaningful use drives more effective use of EHRs and the capture of better data, Levy believes there will be more collaboration between clinical professionals and HIM—a natural progression that also will help with a successful rollout of ICD-10.
Initially, this improved access to data and collaboration will equate to higher reimbursement in the short term, Jarvis says, adding that as data become more discrete, the ability to code accurately becomes easier. As broader-based goals regarding patient care and delivery are achieved over the long haul, he notes that reimbursements will level out. “Better treatment avoids the need for readmission, so you save money in the long run,” he says.
The role of HIM professionals is heightened as meaningful use initiatives continue to mature, according to Underwood. “HIM manages, owns, and is accountable for the data in the organization,” she says. “They will need to take a leadership role in terms of developing the best standards in the managing of the data.”
— Selena Chavis is a Florida-based freelance journalist whose writing appears regularly in various trade and consumer publications covering everything from corporate and managerial topics to healthcare and travel.
A Synergistic Approach to Better Outcomes
With so many federal initiatives on the docket, hospitals are challenged by how to allocate the staff and financial resources necessary to meet important deadlines. And while there are many challenges, industry professionals suggest that all the initiatives are designed to work together to deliver more efficient and effective healthcare.
“What we’ve done in each stage of meaningful use is to enable more use of the elements of EHRs,” says Charlene Underwood, MBA, FHIMSS, senior director of government and industry affairs for Siemens Healthcare and a member of the Meaningful Use Work Group. “The expectation is that what we’ve built through stage 2 and stage 3 will give the necessary elements for caregivers to automate what they need for accountable care.”
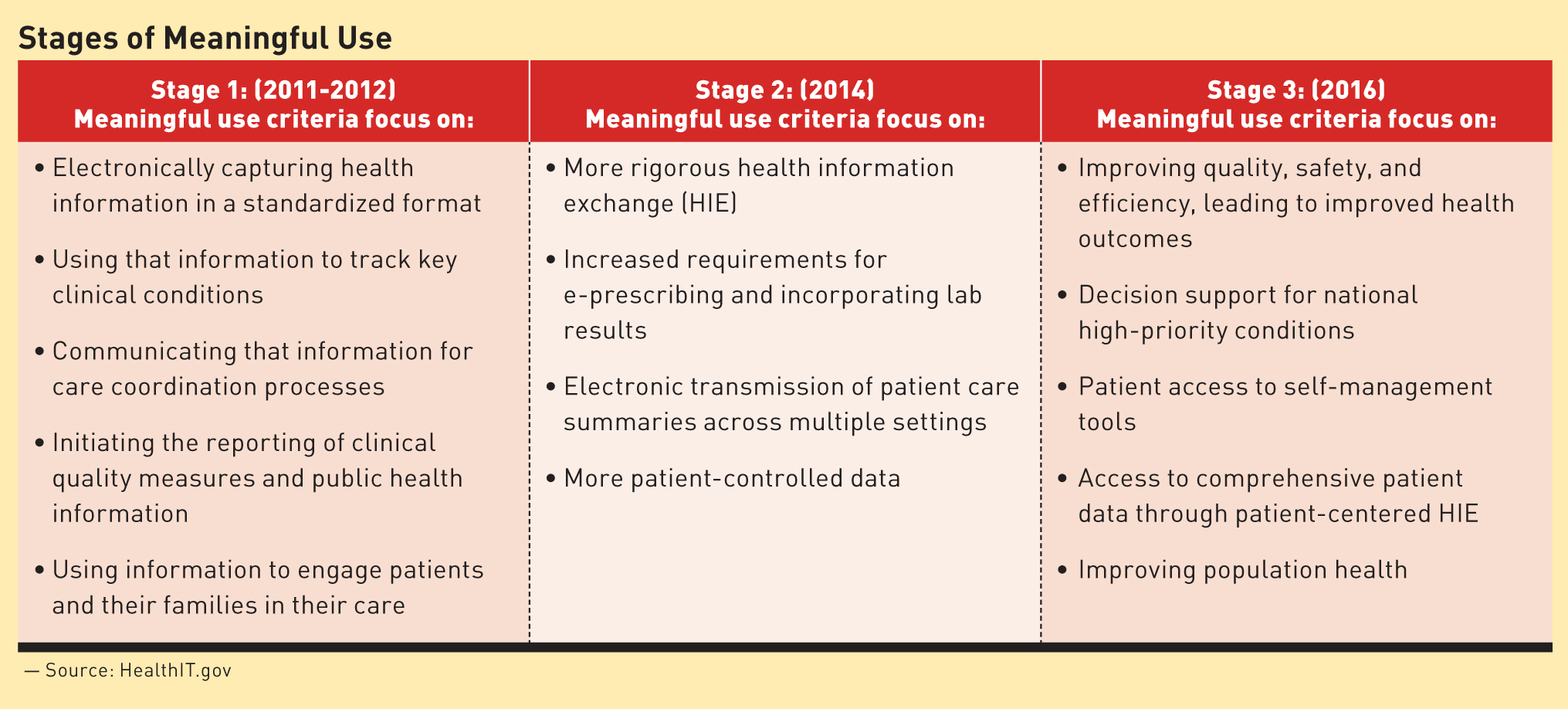
As outlined by Health and Human Services, meaningful use objectives and measures are expected to evolve in three stages, building on one another to achieve the ultimate goal of improved outcomes and better care delivery: stage 1 (2011-2012), data capture and sharing; stage 2 (2014), advance clinical processes; and stage 3 (2016), improved outcomes.
By ensuring EHRs are used in a “meaningful” way, Brian Levy, MD, senior vice president and chief medical officer for Health Language, points out that providers will be better positioned to meet ICD-10 requirements.
“Most providers, up until recently, have been primarily focused on meaningful use. Now they are looking at ICD-10 as an even greater challenge,” he says. “There will be a need for more detailed, granular information, and having an EHR will help accomplish that.”
From meaningful use to accountable care and ICD-10, Levy says, “It’s all about how we better capture data and use it.”
[Click to enlarge image]
— SC