April  2017
2017
Ask the Experts
For The Record
Vol. 29 No. 4 P. 28
Question:
We have an ongoing discussion about this: If the patient has an annual in the clinic and part of the lab work is done in the hospital, the clinic notes state the reason for the visit is the annual. But the lab order from the clinic provider states the only diagnosis is hyperlipidemia and coded E78.5 only, and then the patient calls and says it is coded wrong and that it should be her annual physical.
Can we correct the hospital coding to add the Z00.00 as her primary diagnosis with the hyperlipidemia as secondary in order for her insurance to pay 100%?
I am told "no" because it is diagnostic, but that is not true—it is the same date of service and part of her annual exam.
Belinda Kress-Baruth
Wheaton Franciscan Healthcare
Response:
A physician order is communication from the physician requesting a test be performed. However, the medical record can also be used and must clearly document the physician's intent for the test. The lab could use both the order and the signed encounter note for this exam. The lab must maintain a copy of both pieces of documentation with encounter/lab performed.
Examples of acceptable documentation include the following:
• a signed order by the physician;
• a notation in the patient's medical record documenting the need for or the intent to obtain a specific test, signed by the physician;
• a verbal or telephone order; and
• an e-mail from the physician that must be verified as coming from the physician.
To further address the concerns of the patient with regard to preventive care codes/screening codes vs diagnostic codes: If lab work is ordered or obtained at the preventive care encounter and the patient does not have established diseases or other medical conditions, then screening codes can be used. If a patient has an established disease, the coder would then code both the preventive care/screening code in addition to the diagnosis code as documented by the physician on the order.
Please review payer specific guidelines that would alter the national guidelines for preventive care/screening encounters.
Sources: 42 CFR 410.32 (Code of Federal Regulations), the Centers for Medicare & Medicaid Services' Internet-only Manuals, and Noridian Healthcare Solutions
— Sarah Humbert, RHIA, is a coding and compliance manager and an ICD-10 AHIMA-certified trainer at KIWI-TEK, LLC.
Question:
An 18-year-old patient comes in for an outpatient X-ray of bilateral hands with a diagnosis of age determination and also states the patient is of short stature. Code R62.52 is a pediatric code and is for patients 0–17 years old. What code can we use?
Minerva Martinez, RHIA
Director of HIM
Starr County Memorial Hospital
Rio Grande City, Texas
Response:
The word (child) in the description for R62.52 is in parentheses. This means that the word is a nonessential modifier and is not required to report that code.
There are a few other codes that pertain to short stature due to specific syndromes as well. For example, see E34.3.
If we knew a little bit more about the encounter, we might find a Z code that could also provide an explanation for the service. Consider:
• Z01.89 Encounter for other specified special examinations; and
• one of the codes from the Z02 category.
If we knew more about the case, we might find that these administrative exams might explain the reason for the X-ray.
— Evan M. Gwilliam, DC, MBA, BS, CPC, CCPC, NCICS, CPC-I, QCC, MCS-P, CPMA, CMQP, is chief revenue officer of FindACode.com.
Question:
If an MD (not employed by the hospital) orders a staff nurse (employed by the hospital) to administer moderate sedation, can the hospital report the new moderate sedation codes? If so, which set should be used in this scenario: 99151–99153 or 99155–99157?
Lisa Boyer
Director of Physician Coding Operations
iMedX, Inc
Response:
A facility can code for the facility component of moderate sedation. Moderate sedation is assigned status indicator N, which means it is a packaged service. There will not be separate reimbursement for the service, but you would report it on the claim to account for the services provided to the patient during the outpatient encounter. If the physician is performing the procedure or test requiring the moderate sedation and using a nurse employed by the hospital as a trained independent observer, you would report codes from 99151–99153 depending on the patient age and total time for the moderate sedation.
— Raemarie Jimenez, CPC, CDEO, CPB, CPMA, CPPM, CPC-I, CANPC, CRHC, CCS, is vice president of member and certification development at AAPC.
Question:
This guideline is off the Centers for Medicare & Medicaid Services website. The guidelines in front of the 2017 codebook are from 2016. The book was printed before the guidelines were complete.
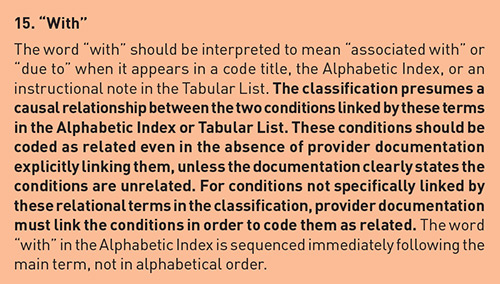
Please clarify the above guideline. Does this mean that if a patient has diabetes and chronic kidney disease, I can use the combination code of E11.22 & N18.-, without the physician documenting diabetes mellitus and chronic kidney disease? I believe I can.
Carmela Giovannini
Response:
I agree that there has been some confusion about this guideline and whether a combination code can be used despite the absence of the provider documentation indicating a link between the two disorders.
According to AHIMA and the American Hospital Association Coding Clinic first quarter 2016 page 11, the subterm "with" in the index should be interpreted as a link between diabetes and any of the conditions indented under the word "with." The physician does not have to indicate linking language between the two conditions to use a combination code.
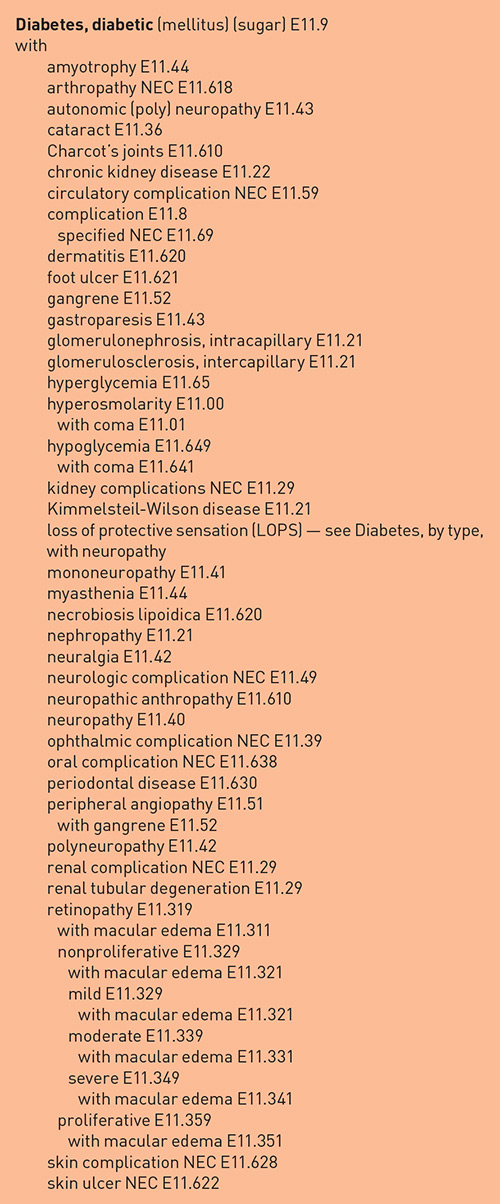
Here is the list of conditions under the subterm "with" for your review.
However, if the physician documentation indicates that diabetes mellitus is not the underlying cause of the other condition, then that condition should not be coded as a diabetic complication, and a combination code should not be used. If the documentation is not precise—and clarity is necessary—then a query should be sent to the provider.
— Valerie Fernandez, MBA, CCS, CPC, CIC, CPMA, is a manager of coding client program development for H.I.M. ON CALL, Inc, and an AHIMA-approved trainer for ICD-10-CM and PCS.



