March 3, 2008
 Coding for Malnutrition
Coding for Malnutrition
For The Record
Vol. 20 No. 5 P. 27
Protein-calorie malnutrition occurs when an individual does not receive adequate protein or calories for normal growth, body maintenance, and the energy necessary for ordinary activities. Geriatric patients are more likely to develop malnutrition than younger patients and are therefore more susceptible to health problems related to an inadequate diet.
The specific ICD-9-CM code assignment for malnutrition will depend on the type and severity, as well as physician documentation. The following are the code assignments for the most common types of malnutrition:
• 260, Kwashiorkor — a severe type of malnutrition characterized by skin and hair pigment changes, edema, and slow growth. Code 260 includes nutritional edema with dyspigmentation of skin and hair.
• 261, Nutritional marasmus — characterized by severe tissue wasting, loss of subcutaneous fat, and often dehydration. Code 261 also includes severe calorie deficiency and severe malnutrition, not otherwise specified.
• 262, Other severe protein-calorie malnutrition — includes nutritional edema without mention of dyspigmentation of the skin and hair.
• 263.0, Malnutrition of moderate degree
• 263.1, Malnutrition of mild degree
• 263.2, Arrested development following protein-calorie malnutrition
• 263.8, Other protein-calorie malnutrition
• 263.9, Unspecified protein-calorie malnutrition
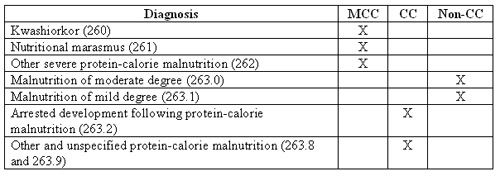
Effective October 1, 2007, a major revision of complication and comorbidity (CC) conditions took place. All ICD-9-CM codes were separated into three categories: a major CC (MCC), a CC, or a non-CC. The following table identifies which category the malnutrition codes belong to:
Conditions that may cause malnutrition include Crohn’s disease (555.9), short bowel syndrome (579.3), malabsorption syndrome (579.9)—or 579.3 if following gastrointestinal surgery—severe burns and injuries, systemic infections, and cancer. Eventually, malnutrition may lead to fatigue; an increased risk of digestive, lung, and heart problems; an increased risk of pneumonia and other infections; anemia; muscle weakness; blood clots; bed sores; and depression.
Diagnosis
Clinical appearance, dietary history, and anthropometry confirm a malnutrition diagnosis. Anthropometry is the measurement of the patient’s age, sex, weight, height, and skin folds. Malnutrition may be classified by calculating weight as a percentage of expected weight and height for the patient’s age and sex. Arm circumference and triceps skin fold measurements will also be below standard. Laboratory findings will show decreased albumin and/or prealbumin levels, with the prealbumin level being a better measurement of malnutrition because it is closest to real time; decreased protein levels; decreased blood urea nitrogen; moderate anemia; and decreased urinary excretion of urea due to decreased protein intake.
Treatment
Initial treatment involves restoring fluid and electrolyte balance. The preferred treatment is oral feeding of high-quality protein foods, especially milk, and protein-calorie supplements. A patient may need supplementary feedings through a nasogastric tube or total parenteral nutrition through a central venous catheter.
Coding and sequencing for malnutrition are dependent on the physician documentation in the medical record and application of the Official Coding Guidelines for inpatient care. Also, use specific AHA Coding Clinic for ICD-9-CM and American Medical Association CPT Assistant references to ensure complete and accurate coding.
— This information was prepared by Audrey Howard, RHIA, of 3M Consulting Services. 3M Consulting Services is a business of 3M Health Information Systems, a supplier of coding and classification systems to nearly 5,000 healthcare providers. The company and its representatives do not assume any responsibility for reimbursement decisions or claims denials made by providers or payers as the result of the misuse of this coding information. More information about 3M Health Information Systems is available at www.3mhis.com or by calling 800-367-2447.



