April  2020
2020
Chart Conundrums: What’s Driving the CDI Resource Crunch? — Alternative Options for Extending Your CDI Team
By Maureen Kelly and Fred Wulf
For The Record
Vol. 32 No. 3 P. 6
Health care reimbursement models continue to evolve, requiring providers to scrutinize clinical documentation to ensure it includes the right content, level of detail, and clarity to support impeccable quality, accurate reimbursement, and downstream care delivery. As a result, clinical documentation integrity (CDI) programs are growing in scope, driving higher demand for CDI specialists to meet new quality and financial challenges such as the following:
• Outpatient CDI Pressures: Payers have begun to shift care delivery to outpatient settings, where documentation review must occur within very short timeframes. Most organizations don’t have outpatient CDI resources in place, which often results in a patient story with gaps and integrity issues.
• Physician Coding Requirements: Physicians face significant new documentation requirements, such as a strong emphasis on medical necessity and hierarchical condition codes, in order to obtain full payment for services rendered by both providers and hospitals.
• Future Reimbursement Cuts: Experts predict reimbursement reductions of up to 25% across all care settings, causing further pressure on revenue cycle teams to ensure care delivery is completely and accurately documented to support high-quality coding and clean claims.
As the demand for CDI specialists grows, revenue cycle leaders find themselves in a crunch. Budgets may limit their ability to hire enough CDI staff to support their program. At the same time, their balance sheets demand that they take steps to eliminate revenue leakage (through improved documentation, coding, and denials management). To remain financially viable, solving the root cause of reimbursement issues at the documentation stage is imperative.
Let’s examine the three market drivers that affect a health care organization’s CDI resource pool: availability, cost, and delivery speed.
Availability of Trained Professionals
While schools and training centers are producing a steady stream of coders, the pool of experienced, clinically trained CDI resources is wanting.
CDI leaders typically develop teams using a combination of two methods. First, hiring CDI staff directly or through consultants is one of the fastest ways to gain the necessary resources. However, with reimbursement cuts looming, that strategy may be financially feasible for only short-term/high-need situations.
The second method involves converting existing coding or nursing staff into CDI specialists by providing additional training. While potentially solving one problem, this strategy presents the following three new issues:
• Effective CDI professionals generally have clinical experience—working on the floor and interacting with patients and physicians—a skill set that most coders don’t possess.
• Highly skilled coders, who may be candidates for CDI work after some clinical training, are already in demand in their current roles.
• If a nurse or a coder receives training and gains CDI certification, they may leave the organization because they can garner a higher rate elsewhere.
As an alternative, CDI leaders are looking to outsourced CDI resources in geographies such as the Philippines. There, an abundance of nurses, medical school graduates, and other health care professionals combine their clinical skills (often having worked in US hospitals during their career) with CDI training and certification to deliver CDI services securely, promptly, and remotely.
In a recent CDI Strategies article, Tonia Catapano, RN, CCDS, director of coding at Yale New Haven, noted, “One of the biggest benefits to adding outsourced CDI staff members to your team is that it allows the department to pilot reviews in other settings and figure out the next best step for expansion without stretching full-time staff too thin or paying for full-time employee salaries right off the bat.”
Highly Competitive Rates
Staffing and costs are perhaps the top challenges facing CDI directors. Before creating or expanding a program, it helps to examine the options. Permanent or temp? Full or part time? Employee or consultant? Onshore or offshore?
Answering these questions can generate an understanding of the cost structure.
Because CDI specialists with clinical experience are in strong demand, opportunities to hire US-based staff directly are very limited, very costly, or both.
According to a recent Association of Clinical Documentation Integrity Specialists survey, the annual pay rate for (the majority of) CDI nurse specialists ranges between $70,000 and $89,000, not including benefits. Salaries can increase to more than $100,000 in rural areas where resources are especially limited. Annual certified coder salaries average between $30,000 and $79,500 and significantly increase following CDI training and certification.
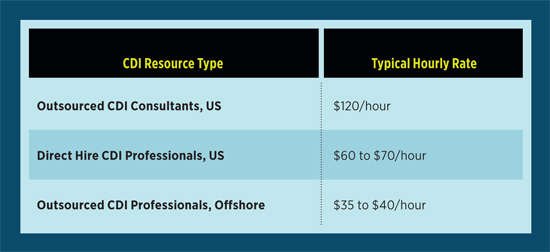
At an average of $120 per hour, enlisting help from a CDI consultant is even more costly (See chart).
Hiring full-time employees can build knowledge and create consistency within your CDI program. However, along with consultants, they come with a hefty price tag. You can also expect to continually compete against other health care organizations to keep that talent on your team. As your CDI program evolves, it’s important to weigh the benefits delivered by CDI staff in terms of clean claims and accurate reimbursement against the compensation costs.
Ramp-up time also has a cost. Whether an organization’s personnel strategy includes US-based nurses with CDI credentials, converting existing coders to full-time CDI positions, or partnering with an offshore provider for CDI services, every new CDI team member requires a similar ramp-up path. This journey includes a training period, some facility-specific education, and intensive quality monitoring for 30 to 60 days to ensure compatibility with a CDI program.
Speed and Responsiveness
Rapid CDI review turnaround time is essential, especially in a high-volume environment such as today’s outpatient settings. Providers are stretched thin trying to meet the needs of increasing patient volumes. Fast-paced, short outpatient encounters leave minimal time for concurrent review and follow-up queries related to medical necessity of care, hierarchical condition codes and risk adjustment, charge capture, and professional billing.
To support accurate and timely billing, prospective reviews (after the patient is scheduled but before the patient encounter) are often the key to a successful outpatient CDI program. Inpatient CDI teams—employees and consultants—generally work traditional work hours, making staffing outpatient programs a challenge. Depending on their availability, existing CDI professionals may be willing to shift to evening or weekend work for a slightly higher rate. Alternatively, offshore vendors offer timely, overnight review as a standard service due to the variation in time zones.
The Rise of First-Level CDI Review
To resolve the CDI crunch, health care leaders must determine how they can best deploy their existing resources across an array of evolving review requirements, care settings, and quality programs. Using an outsourced team, typically located offshore, for first-level CDI review can be a valuable element of a successful strategy. What is it, and how does it work?
• Outsourced CDI specialists perform a standard review, confirming documentation completeness and accuracy, flagging issues, and identifying necessary queries (if any) for the record.
• Because offshore teams typically perform the work during the overnight hours in the United States, the first-level reviews are completed before the start of each business day—a considerable benefit for both inpatient and outpatient facilities.
• Facility-based CDI staff receive the reviewed record and related notes and comments. They quickly assess the review findings and either approve the record or make any necessary edits or queries.
• Depending on the facility, queries can also be submitted by first-level reviewers to providers electronically overnight for their response in the morning.
First-level review is a common practice in a variety of industries, including the legal sector where discovery assets, contracts, and other critical business documents require efficient comprehensive review.
Due to the repetitive nature of care types and the low level of case complexity, outpatient health care settings are a natural venue to deploy first-level reviewers. Deploying these teams allows “in-house” CDI specialists to manage reviews more efficiently, use their time to focus on higher-dollar, more complex cases, and support CDI programs in other areas of the organization. Inpatient settings also can benefit from establishing a first-level review stage in their CDI processes, enabling local CDI staff to focus on managing physician queries and education to generate long-lasting quality improvement.
As organizations such as Yale New Haven already know, working with offshore CDI resources can ease personnel pressures and reduce the overall cost of CDI programs while maintaining quality standards and supporting an efficient revenue cycle.
— Maureen Kelly is vice president of health care at EXTEND Resources.
— Fred Wulf is director of operations at EXTEND Resources.



