June  2015
2015
Copy and Paste: Don't Mess Up a Good Thing
By Robert S. Gold, MD
For The Record
Vol. 27 No. 6 P. 10
Once upon a time, long ago in a galaxy far, far away, physicians wrote history and physicals (H&Ps) and progress notes and consults and discharge summaries. Then, dictation and transcription became the preferred documentation method. Finally, the industry became digital, introducing professionals to a world of templates and checkboxes in which even scribes could perform chart entry.
Throughout all these permutations, no matter the setting, whether teaching environments, private hospitals, or clinics, professionals often are on hand to take care of chart entry when the treating physician doesn't take primary responsibility. They may be residents, nurse practitioners (NPs), or physician assistants (PAs)—even physicians practicing without a US license and registered nurses are dictating discharge summaries.
Some physicians cosign or electronically sign the notes created by these professionals—and subsequently bill for the patient visit. They may or may not have seen the patient. They may or may not have examined the patient. Nevertheless, the documentation consisted of a real or electronic signature on someone else's work. Guess what? For all intents and purposes, it's fraud. The physicians may have done everything correctly, but the evidence shows only another person's work. As a result, physicians lean on copy and paste—and bill based on someone else's work. At least, that's what it looks like.
Is this an overreaction? Is it a hysterical perspective? Not necessarily. Is every physician guilty? Certainly not. They all try to see patients while managing the documentation foibles associated with EHRs. Nevertheless, it's happening, and it's been going on since paper records were the dominant documentation method. In an electronic environment, it's easier to fall prey to this practice, causing some physicians to become careless to the point that they believe they can get away with it or not be in self-protective mode.
A Brief History
In December 1995, the University of Pennsylvania, without admitting wrongdoing, entered into a voluntary settlement with the Department of Justice to pay approximately $30 million in disputed Medicare billings. According to the Government Accountability Office, (GAO) the settlement stemmed from an Office of Inspector General audit that concluded that some of the university's teaching physicians had inappropriately billed Medicare because medical records did not adequately document their involvement in services provided by residents. The audit also determined that some teaching physicians had upcoded their claims, billing for more complex and expensive services than may have been provided.
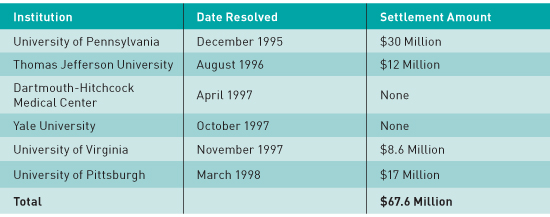
According to the GAO, notable settlements from pre-2000 include the following:
In September 2012, Health and Human Services and the US Attorney General's office warned providers about misusing the copy-and-paste function in EHRs. "Law enforcement will take appropriate steps to pursue health care providers who misuse electronic health records to bill for services never provided," the letter stated. The conclusion was that if there's no evidence that the work was performed, "we are under no obligation to pay you."
The ease in which volumes of laboratory and radiographic data can be imported into consults and diagnosis lists and be reproduced to depict a patient's 50-year medical history into a note for a two-day hospital stay lends itself to potential abuse.
Patients at Risk
Unless health care organizations standardize physician documentation procedures and limit the amount of copy-and-pasting, they run the risk of notes becoming "bloated" and patient safety being compromised, Jody Cervenak, principal of HIT consulting firm Aspen Advisors, told attendees at last year's College of Healthcare Information Management Executives Fall CIO Forum. "It's been challenging for both doctors and health care systems in general … to produce a document that reflects the patient story in the most concise, complete, and informational way," she said.
Cervenak quoted 17th-century French mathematician and philosopher Blaise Pascal, who wrote, "I have made this letter longer than usual, only because I have not had the time to make it shorter," according to Healthcare IT News.
Progress notes have gotten progressively longer, less informative, and, in some cases, laden with misinformation due to the propagation of obsolete clinical data obtained during the process of copying forward. In fact, the indiscriminate use of copy forward has led to several patient safety issues can tarnish the credibility of an entire note. For example, a note may state that a patient has a surgery scheduled despite the fact that it already had been performed. Shoddy documentation can reflect poorly on physician care should the note be introduced in a malpractice lawsuit.
When documenting electronically, it's convenient to copy forward reams of data from prior notes in an effort to be both comprehensive and speedy. There's also a misconception that chronicling all data (including lab data) improves the substantiation of higher evaluation and management codes for physician billing purposes. Over time, this practice leads to note polymerization, rendering it increasingly difficult to extract essential information from a haystack of irrelevant and obsolete narrative.
Current Picture
I have visited numerous hospitals in various stages of transitioning to an EHR. Teaching hospitals have their particular sets of problems as do community hospitals with rotating residents. At community hospitals, staff members believe residents are caring for patients and handling documentation during morning rounds. Some attending physicians are under the impression they only have to sign the resident notes to bill for the H&P, daily rounds, and the discharge visit. But plugging in an electronic template that reads "I was present during the resident visit and agree with the above" is not sufficient. Some even copy and paste previous resident notes into today's note.
These actions are noncompliant and can lead to costly audits and patient harm.
At hospitals with hospitalist services, questionable documentation takes several forms, including an emergency department (ED) physician's note copied and pasted into the H&P and the evening progress note being an exact match of the H&P. Other discrepancies occur when the twice-a-day visits contain the same verbal content as well as increasing volumes of lab results and radiographic reports. In addition, a patient may be discharged with a note to "transfuse a unit of PRBCs [packed red blood cells] tomorrow" (the transfusion actually was given eight days ago) and walk out of the hospital on oral meds with sepsis, currently in septic shock, acute respiratory failure, and acute kidney injury still documented as being active diagnoses.
In that case, there's no evidence of medical decision making after the ED visit. In addition, there's no indication whether the patient recovered and that pneumonia was ruled out when an order was given to discontinue antibiotics. As a result, the chart receives an incorrect code for pneumonia.
Hospitals with hospital-employed NPs, PAs, and foreign medical graduates present unique issues. Physicians can bill office or hospital visits in which their employed nurses, NPs, and PAs perform certain tasks so long as the physician completes and validates the work. When credentialed PAs and NPs are used, physicians can bill 80% of the visit charge.
However, if the NP, PA, or foreign medical graduate is hired by the hospital, physicians cannot bill for any portion of the practitioner's work. Only if the practitioner is a physician extender in their practice can physicians bill for the care rendered. Keep in mind that hospital- and office-hired nurses cannot perform complete H&Ps and have the physician countersign or make additions. Registered nurses are not independent practitioners with medical staff privileges to complete an H&P exam.
While office-hired nurses can complete sections of the history of present illness, medical history, and review of systems in a hospital setting, hospital-hired nurses cannot because they're not part of the medical staff. Thus, it's incorrect for physicians to copy and paste and sign their work. Perhaps most disconcerting is when practitioners complete discharge summaries having never seen the patient. In these circumstances, dictation often occurs after code assignment, resulting in coder language becoming part of the discharge diagnosis list (meaning the coder is diagnosing the patient).
And physicians bill for such visits?
— Robert S. Gold, MD, is cofounder of DCBA.



