September  2019
2019
Inside Interoperability: Is TEFCA 2.0 — Finally — the Harbinger of True Interoperability?
By Bruce Lawrence
For The Record
Vol. 31 No. 8 P. 28
On April 19, the Office of the National Coordinator for Health Information Technology (ONC) released the long-awaited second draft of the Trusted Exchange Framework and Common Agreement (TEFCA), a proposed strategy mandated by the 21st Century Cures Act of 2016 that provides the industry with the policies and standards necessary to enable true data interoperability and exchange of patient data.
According to ONC, Draft 2 of TEFCA “is designed to scale EHI [electronic health information] exchange nationwide and help ensure that HINs [health information networks], health care providers, health plans, individuals, and many more stakeholders have secure access to their electronic health information when and where it is needed.”
Based on my time as the CEO of a large US health system, I understand the enormity of the challenge. A health system’s focus is always to provide high-quality care to patients—and there are obviously some strong benefits to having shared, accessible information. Having inaccurate, incomplete, and unactionable data acts as a barrier to that goal, and I believe TEFCA holds great promise to break down those barriers.
The ability to share and access information across all health care channels, as TEFCA demands, would dramatically improve care coordination. It would bring providers, patients, and caregivers together, resulting in more robust, complete, holistic care. And it also has the potential to increase efficiency while reducing costs.
For example, providers order duplicate tests far too often because there is no easy way to access patient health information if the patient has recently moved or changed providers. These sorts of unnecessary tests and procedures are not only financially burdensome to patients and payers but they may also actually increase risk and diminish patients’ emotional well-being, which can negatively impact outcomes as well.
If TEFCA could help overcome a portion of these kinds of financial and emotional challenges, then its benefits would be enormous.
However, as history has taught us when facing daunting challenges—from politics and social structures to the battlefield—what works in theory doesn’t always play out as planned in practice unless it’s executed thoughtfully and strategically and with an ability to adjust in real time based on changing circumstances.
Barriers to TEFCA’s Success
As hospitals, health systems, and payers prepare to comply with the guideposts outlined in TEFCA and meet Health and Human Services’ larger push for interoperability head on, they’ll need to have complete, enriched, actionable data—and solid data governance practices—in place in order to effectively share large volumes of data from multiple sources.
At this point, health care organizations are facing serious financial and technological burdens that, if not addressed, will act as barriers to rapid, effective compliance.
According to a report from the American Hospital Association (AHA), there are five top barriers to data exchange and interoperability (see diagram below).
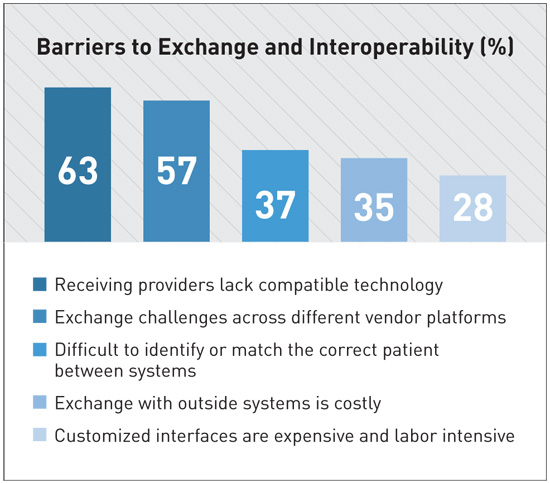
All of these barriers are very real problems that health care organizations face every day. Each must be addressed before TEFCA compliance is possible. And we’re not there yet.
According to an ONC analysis of 2017 data from the AHA’s Information Technology Supplement survey, despite the fact that 93% of acute care hospitals have upgraded to or plan to adopt the most recent EHR standards, the number of hospitals able to integrate data is still at only about one-half (53%). “Only 4 in 10 hospitals reported they can find patient health information as well as send, receive, and integrate patient summary of care records from sources outside their health system,” the analysis notes. “Engaging in all four interoperability domains is critical to ensuring that clinicians have information they need at the point of care.”
Simple data exchange is not enough to overcome these hurdles. What we need is “data enrichment,” which encompasses so much more than “data management.” We need technology and business strategies that take into account data extraction, standardization, normalization, and identity management, leading to actionable business decisions that allow organizations to deliver on a wide variety of use cases.
The bottom line is, just because data are being transmitted under legal guidelines such as those outlined in TEFCA, that doesn’t mean that the data being transported are high quality and complete, or that they’re being delivered in a way that is usable and actionable.
An Interoperable Future
There’s no doubt that interoperability is on the way, or that it’s necessary. What remains to be seen is how we can get there. Strategic, thoughtful processes and the right technological capabilities are integral to our collective success.
The College for Healthcare Information Management Executives (CHIME) supports the idea of a slow and measured approach. In a recent letter to the Centers for Medicare & Medicaid Services and ONC, CHIME stated, “Our members strongly support an interconnected health care system whereby clinicians have timely access to the medical records and necessary patient information at the point of care. … [There is] a need to thoughtfully sequence certain components such that: 1) vendors and providers have adequate development time; 2) greater upfront emphasis is placed on building provider capacity to utilize data received; and 3) ensuring adequate outreach and education initiatives are provided to providers and patients.”
In fact, many industry stakeholders are recognizing that a strategic approach that takes technology and data quality into account is the best way forward. “We have significant concerns that the proposed implementation timeline fails to recognize both the operational complexity associated with building the required technology and the lack of mature standards for the proposed data elements and exchange,” America’s Health Insurance Plans said in its public comment on the rule.
And the AHA report notes, “The ability to communicate vital health data is necessary to realize the full potential of our nation’s system of health care. … For the best outcome, it is imperative that accurate, standardized, accessible, and exchangeable health information from all sources accompany patients every step of the way. … We are inching closer to, but still short of, the ideal of seamless interoperability.”
As someone who is intimately familiar with the ongoing struggle of providing high-quality, coordinated care to patients, I couldn’t agree more.
— Bruce Lawrence is the former president and CEO of INTEGRIS Health (Oklahoma’s largest health care system) and current board of directors advisor for data enrichment and integration technology company Verinovum. He can be reached at bruce_lawrence@outlook.com.
TEFCA NEWS TIMELINE
• December 13, 2016: The 21st Century Cures Act is signed into law, designed to help accelerate medical product development and bring new innovations and advances to patients who need them faster and more efficiently. Part of the Cures Act is a mandate to define standards for data interoperability.
• January 2018: The Office of the National Coordinator for Health Information Technology (ONC) releases the first draft of the Trusted Exchange Framework and Common Agreement (TEFCA), which is intended to meet the mandate that was part of the Cures Act, for public comment.
• April 19, 2019: ONC releases the long-awaited second draft of TEFCA, part of the 21st Century Cures Act that was first introduced in 2016.
• May 22, 2019: The Health IT Advisory Committee (HITAC), a government group established under the 21st Century Cures Act to advise ONC, finalizes its recommendations on the proposed TEFCA ruling. HITAC recommendations include implementing a two-tiered payment system to help IT vendors with interoperability-associated costs, removing price transparency stipulations, and eliminating the data segmentation for privacy provision that would allow patients to pick and choose which elements of their health record providers can access.
• July 23, 2019: The ONC puts out a request for public comments on the Interoperability Standards Advisory, “a dynamic, coordinated catalog of the standards and implementation specifications that can be used to meet interoperability needs in health care,” which “continues to serve as the industry’s primary source of input on the interoperability standards that are a best fit for a particular health information technology use case, and plays a key role in ONC’s efforts to implement the 21st Century Cures Act.” The comment period closes September 23.
— BL



