Fall  2023
2023
Risk Adjustment: Seven Critical Factors for a Successful Risk Adjustment Program
By Eric McGuire
For The Record
Vol. 35 No. 4 P. 10
Risk adjustment models such as hierarchical condition category (HCC)—so named because the highest severity in the family or related category trumps less severe conditions—deliver critical transparency not only in patient care and outcomes but also in forecasting costs of that care between payer and provider organizations.
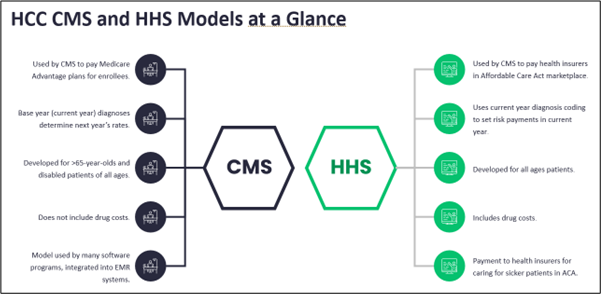
A statistical method used to predict someone’s likely use and costs of health care services, risk adjustment, is used by CMS to determine and adjust capitated payments for Medicare Advantage (MA) plans. Health and Human Services also utilizes the model with the Affordable Care Act Marketplace and other value-based care plans—which are expected to make up 60% of all payer contracts by 2028—to provide insights into patient health and care across payers and providers. Risk adjustment is also used across all payment models to promote better management of patients with multiple chronic conditions.
How It Works
Risk-adjusted models like HCC are enjoying skyrocketing popularity. This is particularly true for MA plans, which now cover 48% of all Medicare beneficiaries—a growth of 2.7 million since 2022. During that same timeframe, enrollment in original Medicare declined by 1.3 million as consumers flocked to MA plans’ lower copayments and out-of-pocket maximums. There’s also a greater variety of MA plan benefits, allowing consumers to shop for the plan that meets their specific financial and care needs. All of this is driving the steady growth of enrollment into MA plans that are expected to extend across the next decade.
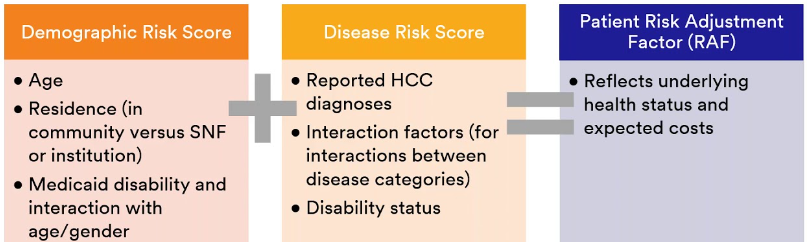
HCC models leverage risk adjustment factors, or RAF scores, to determine the estimated cost of an individual’s care based on their disease burden and demographic information, including age, gender, socioeconomic status, disability status, insurance status, and/or institutional status. Each HCC associated with a patient is assigned a relative factor that’s averaged with any other HCC code factors, as well as a demographic score. HCC RAF scoring uses an additive approach, meaning the scores for various HCC conditions are added up to provide the composite RAF score.
There are numerous benefits of risk adjustment or HCC coding, including its ability to predict a person’s future health care utilization and costs and the transparency in patient conditions it creates between payer and provider. It also ensures adequate compensation for health plans and payers, helps provider organizations develop strategies and forecast costs to support patient populations, and provides a mechanism to ensure providers are compensated fairly for the patients they manage. Finally, risk adjustment models enable more accurate reimbursement by accounting for differences in patient demographics and other risk factors that affect outcomes outside of the provider’s control.
Seven Factors for Success
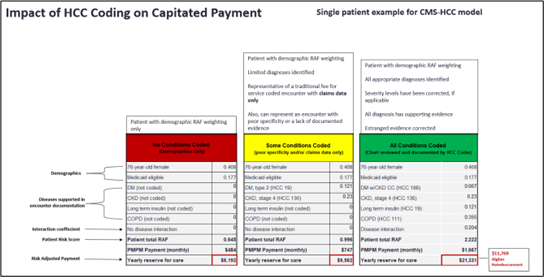
For providers, finding ways to develop or improve their risk adjustment programs is critical, as is avoiding mistakes that can significantly influence health outcomes for the organization’s patient population and its financial well-being—particularly considering that a 0.1 improvement in a patient’s RAF score equals a 10% increase in Medicare payout.
To that end, the following are seven critical factors to consider when setting up risk-adjusted or HCC programs.
1. Prospective review models, especially those that utilize a postencounter (concurrent) update process, are a better option than standard retrospective reviews, in which medical notes, previous coding, and additional ancillary and other reports are audited after the fact to ensure all diagnoses have been captured and that any no longer applicable are removed. These certainly have a role to play in risk-adjusted coding models, but a more powerful auditing tool is the prospective review.
Conducted by clinical documentation integrity (CDI) specialists, these are reviews of the medical record and findings from retrospective and postencounter reviews with the goal of preparing the provider for the patient’s annual visit. In addition to reviewing the medical chart to identify proactive queries and severity of illness considerations, the CDI specialist will reevaluate retrospective findings that affect severity, missing diagnoses, and other potential diagnoses. When appropriate, it can be narrowed to focus more deeply on specific areas (eg, kidney, behavioral, and diabetes). Findings from the prospective review, which ideally should take place within four weeks of the patient’s annual visit, are then compiled into a report for the provider to use as checklists for those annual visits.
2. There are specific requirements for the annual visit that need to be carefully documented. Because individual HCCs are valid for just one year, it’s imperative that patients with chronic conditions have an annual visit with their primary care providers. During this visit, the condition(s) should be discussed and documented for the appropriate HCC code to be reported for the new year and considered in establishing the patient’s RAF score.
3. Overall population health factors are significant factors in payments for Medicare contracts. Using risk-adjusted coding to align health care services to the unique needs of a patient or member population is critical for success under these models. Doing so provides deeper insights into the factors involved in preventive and acute care and available treatment options. This allows payers with MA plans to forecast costs across member risks, while providers can better target investment dollars into services that align with the overall patient population’s needs. For example, a hospital in Utah, where lung cancer rates are lowest, would invest oncology service dollars far differently than would one in Kentucky, where they are the highest.
Finally, risk adjustment allows payers to determine the average costs of care for their entire member population in a particular community or region, which allows the establishment of appropriate premium or payment amounts, while providers can justify being reimbursed at the highest appropriate levels based on the amount of time they project they will spend with each patient based on cross-conditions and/or the presence of multiple chronic conditions.
4. Performance metrics should be focused on the accurate selection of all the diagnoses in a patient’s medical history, most of which would be missed in a scenario where measurements are based solely on claims data. This will require a comprehensive retrospective review of patients’ health histories to include documentation from all the providers they’ve seen—for example, ancillary, lab, and radiology reports—to ascertain the most accurate picture.
5. Problem lists can be problematic. The problem with problem lists is that they are rarely well maintained, which means they are likely to contain clinical data that’s no longer supported by evidence or is no longer applicable. Thus, while problem lists can be a reference tool, they should not be relied upon too heavily when coding for HCC categories to avoid working from inaccurate or outdated information that will result in a denial.
6. HCC workflow tools improve productivity and accuracy and will improve RAF scoring. Leveraging workflow tools like computer-assisted coding, CDI, and HCC tools can help ensure the highest appropriate code is selected based on documentation and other pieces of evidence within the patient’s record. These tools ideally will leverage natural language processing and machine learning to review, annotate, and highlight if evidence is missing or outdated and to pull in or suggest more appropriate codes.
It’s important to keep in mind that HCC is not about coding. Rather, select ICD-10 codes are mapped to the appropriate HCC category, which is determined based on the evidence that’s collected and using CMS forms that allow up to 12 diagnoses to be listed. Those must then be verified, validated, and mapped before submission to the payer. The right workflow tools streamline this process, boosting productivity and ensuring no evidence is overlooked.
7. Risk adjustment analytics improve care and reimbursement. Properly performed risk adjustment analytics as determined in part by a deep retrospective review ensures that all appropriate diagnoses are identified and utilized to help determine that a patient has access to the proper types and levels of care needed for optimal outcomes—and that the provider and payer receive the highest appropriate reimbursement for managing that patient’s care. This includes both the demographic (age, residence, and Medicaid disability and its interaction with age and gender) and disease risk (reported HCC diagnoses, interaction factors between disease categories, and disability factors) scores that make up the patient’s RAF score.
Conclusion
HCC and other risk-adjusted models are enjoying a surge in popularity for their ability to project health care utilization and costs and the unprecedented transparency they create between payers and providers. This, in turn, ensures appropriate reimbursements for both and helps providers invest in the types of clinical services that align with their specific patient population’s needs.
Designing mistake-proof risk adjustment programs is critical, as the stakes are high in both human and monetary costs. The good news is that arming themselves with the proper tools and understanding the rules of participation can set provider and payer organizations up for success in today’s value-based world.
— Eric McGuire is senior vice president of medical coding and clinical documentation improvement service lines and corporate strategy at AGS Health (www.agshealth.com).



