Spring  2023
2023
Coding Corner: Evaluation and Management Guidelines 2023
By Roee Kenett, MD
For The Record
Vol. 35 No. 2 P. 30
Taking a Closer Look at Coding and Documentation Changes in Emergency Medicine
Medical coding and documentation significantly contribute to the high level of administrative burden and expenditure in health care across the United States. Physicians spend hours of their day on documentation, navigating a maze of complex, ever-changing guidelines to accurately report patient encounters.1 Medical coders must then analyze the documentation and sift through thousands of medical charge codes to accurately code each patient encounter and ensure the appropriate reimbursement. The complexity involved with both documentation and coding processes creates room for errors that can lead to denied medical claims, audits, and serious financial losses for health care providers. In the wake of the COVID-19 pandemic, these challenges have become even more prevalent with health care staff in short supply and health systems operating on razor-thin margins.2,3
The need to address the challenges associated with medical coding and documentation has not gone unnoticed. On July 1, 2022, the American Medical Association (AMA) released significant revisions to evaluation and management (E/M) guidelines, including the first changes to emergency department (ED) E/M guidelines in more than 25 years. This latest version, “E/M 2023,” includes a number of coding and documentation guideline changes aimed at reducing current administrative burdens faced by health care providers. While the changes are extensive, there are specific measures health care providers can implement in the ED to ensure continuous compliance and make the transition to E/M 2023 guidelines as smooth as possible.
Administrative Complexity Is Unsustainable Operationally and Financially
The Journal of the American Medical Association’s (JAMA) estimates show that the United States spends nearly 18% of its gross domestic product on health care, and that number only continues to rise.4 Research from JAMA also indicates that waste accounts for about 25% of this spending, with “administrative complexity” being the single largest component of health care waste in the country, totaling $265.6 billion of an estimated $760 to $935 billion in waste annually.
Much of the excess overhead can be attributed to tremendous workflow and process redundancies and other low-value, manual, error-prone tasks. When it comes to revenue cycle management in the ED, one of the most costly areas historically has been medical coding. Translating patient records into codes for billing is a complicated, largely manual process. Any issue during the coding process—whether related to complex regulations, lack of resources or qualified staff, or workforce burnout—can lead to costly backlogs and lingering days in accounts receivable and negatively affect reimbursement through underpayments and denials.
To tackle these challenges and drive the high-quality coding that’s critical to ensuring accurate, timely reimbursements, provider organizations have attempted to hire more coders overseas, outsource the entire coding process to independent revenue cycle management companies, and increase the administrative responsibilities of already overworked health care professionals. However, none of these approaches has proven scalable or cost effective. The reality is that even with highly trained and skilled coders in place, the complexity of documentation and coding practices continues to cause significant operational and financial challenges for providers.
Simplifying Coding and Documentation in the ED
While attempts have been made to simplify coding and documentation processes in certain specialties, guidelines for the ED have not been significantly updated in more than 25 years. This changed on July 1, 2022, when the AMA released a number of significant revisions to previous E/M guidelines. Effective as of January 1, 2023, E/M 2023 applies to the ED and other settings such as nursing facilities, home and resident services, and more.
The goals of E/M 2023, as outlined by the AMA’s CPT Editorial Panel, are as follows5:
• decrease administrative burden of documentation and coding and align CPT and CMS whenever possible;
• decrease the need for audits through the addition and expansion of key definitions and guidelines;
• decrease unnecessary documentation in the medical record that is not needed for patient care; and
• ensure that payment for E/M is resource based and that there is no direct goal for payment redistribution between specialties.
To achieve these goals, E/M 2023 includes significant changes to previous ED documentation and coding guidelines. Most significantly, E/M 2023 guidelines outline the elimination of history and physical exams as elements for ED E/M code selection and, beginning in 2023, ED E/M services will be based only on medical decision making (MDM). Additionally, the new guidelines include significant modifications to the criteria for determining the appropriate level of MDM.
Preparing for a Smooth Transition
For health care providers, the need to quickly incorporate such extensive changes complicates the E/M 2023 adoption process. This is especially true for the ED. Physicians, medical coders, educators, and other ED staff involved in documentation and coding processes have been following the same set of E/M guidelines for years and have developed their own internal procedures or practices to ensure the highest documentation and coding standards. An extensive set of guideline revisions, such as those included in E/M 2023, creates room for documentation and coding errors, which can lead to costly denials and underpayments down the line.
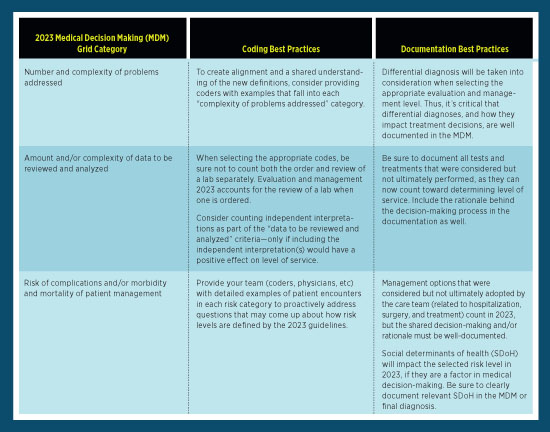
To avoid such errors, there are steps that both physicians and medical coders can take to ensure compliance with the new guidelines. The table below outlines examples of coding and documentation best practices that can help ensure a smooth transition to E/M 2023.
Looking Ahead to E/M 2023’s True Impact in the ED
It’s now been several months since E/M 2023 guidelines went into effect. As health care providers adjust internal coding and documentation practices to align with new guidelines, it will be interesting to see if and how the original goals of the AMA are met. Will these changes really decrease the administrative burden faced by physicians and medical coders today? Will the new guidelines also impact other areas of health care administration, such as quality and reimbursement? These questions can’t be answered quite yet, but in time and with the right technology and tools, E/M 2023 has the potential to deliver on its goals and meaningfully simplify coding and documentation.
— Roee Kenett, MD, is the medical director at Nym, where he manages Nym’s medical team. In his role, Kenett maintains and develops the clinical knowledge capabilities behind Nym’s medical coding engine and is responsible for ensuring that it achieves maximum coding accuracy. Additionally, Kenett is responsible for adjusting the engine to accommodate specific guidelines and workflow needs of Nym clients. He earned his Doctor of Medicine degree from Tel Aviv University and has a BASc in medical sciences from Ben-Gurion University of the Negev.
References
1. Medscape physician compensation report 2018. Medscape website. https://www.medscape.com/sites/public/physician-comp/2018. Accessed March 7, 2023.
2. The complexities of physician supply and demand: projections from 2019 to 2034. Association of American Medical Colleges website. https://www.aamc.org/data-reports/workforce/data/complexities-physician-supply-and-demand-projections-2019-2034. Published June 2021. Accessed March 7, 2023.
3. National hospital flash report: January 2023. KaufmanHall website. https://www.kaufmanhall.com/insights/research-report/national-hospital-flash-report-january-2023?utm_source=agcy&utm_campaign=kh-nhfr&utm_medium=pr&utm_term=jan-nhfr-230130. Published January 30, 2023. Accessed March 7, 2023.
4. Papanicolas I, Woskie LR, Jha AK. Health care spending in the United States and other high-income countries. JAMA. 2018;319(10):1024-1039.
5. CPT evaluation and management. American Medical Association website. https://www.ama-assn.org/practice-management/cpt/cpt-evaluation-and-management. Updated December 5, 2022. Accessed March 7, 2023.



