Spring  2023
2023
Documentation Dilemmas: Risk Adjustment Factor Methodologies
By Teresa Brown, RN, CCDS, CDIP, CCS
For The Record
Vol. 35 No. 2 P. 5
Planning for the Future
In this ever-changing health care landscape, we’re faced with many challenges, including staffing shortages, staff burnout, struggles with employee retention, supply chain delays, and financial recovery from COVID-19. In light of these difficulties, how do facilities and providers plan for future health care costs?
First, consider the origin of hierarchical condition categories (HCCs). Medicare Advantage (MA) was created by the Balanced Budget Act of 1997. CMS established the Medicare risk adjustment process to modify the amount of remuneration paid to an MA organization for each beneficiary to cover, at a minimum, all the services afforded by traditional Medicare Parts A and B.
CMS pays each MA organization a fixed amount, known as a capitated payment, on a per member per month basis. As a result, all financial risk is shifted from CMS to the MA organization, ie, if a beneficiary uses more health care resources each year than are covered by the fixed payments from CMS, the health plan must absorb the excess costs. To offset any tendency to cherry-pick healthy beneficiaries, CMS adjusts the capitated payments according to the actuarial risk (ie, anticipated health care expenses) of the MA membership. This risk-adjustment process is based on a regression model developed by CMS known as the CMS-HCC model. This model was initially implemented in 2004 by CMS to provide risk adjustment methodologies to commercial Medicare plans—MA. Since 2014, when individuals and small businesses have been able to purchase health plans through exchanges, HCCs have become a significant concern far beyond the traditional Medicare population.
HCCs are used to determine premiums and budgets (not payment) for health care providers and health care plans (payers) with risk sharing agreements—MA, commercial accountable care organizations, and other shared savings programs.
Risk Adjustment Methodology
Risk adjustment is calculated using an actuarial tool that’s been developed to predict the cost of health care for covered beneficiaries/enrollees. The score is determined by using a combination of demographic information along with disease information to predict the cost of future health care for the enrollees of the plan. The score is highest for the sickest patients as determined by the combination of factors. The risk adjustment factor (RAF) is the total score of all relative factors related to one patient for a total year and includes diagnoses, age, living arrangement, and disability status.
The following are sources of data used to calculate the RAF score:
• Diagnoses: Included in current risk adjustment model, valid provider, valid data collection method;
• Providers: Physicians, nurse practitioners, certified registered nurse anesthetists, physician assistants, psychologists, and psychiatrists;
• Provider types: Inpatient hospitals, outpatient hospitals, and physicians;
• Services excluded: Durable medical equipment, laboratory, and diagnostic radiology; and
• Exclusions: Hospice, skilled nursing facility, home health, and free-standing ambulatory surgery centers.
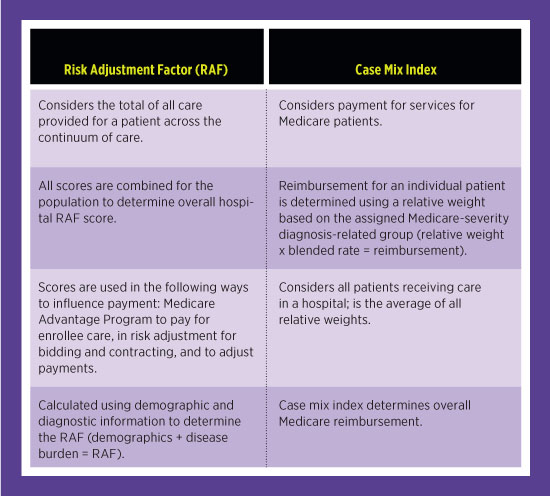
Comparison of RAF to Case Mix Index
It’s important to know the RAF and case mix index scores to accurately reflect the patient population and disease progression.
These are compared in the table below.
Diagnosis Documentation Requirements
It became necessary to report chronic conditions every year as the clock reset on January 1. Diagnoses must be captured in a face-to-face meeting and must be documented in the medical record with appropriate identification, date, and provider signature.
Specific reporting rules include the following:
• Chronic diseases can continue to be reported on an ongoing basis if the condition receives treatment and care.
• Diagnoses that receive care and management during the encounter can be reported.
• Diagnoses that have been resolved or are no longer being treated should not be listed. (Be careful using diagnoses on problem lists that have been resolved.)
• Malignancies can be reported if active treatment continues.
HCC Models
There are several types of HCC models depending on the patient population developed by CMS for risk adjustment of the MA Program (Medicare Part C), based on aged population (older than 65 years). The most well-known are the CMS-HCCs relevant for members in MA Plans. The demographic for this population is the same as that for those in traditional Medicare, and there are nearly 10,000 ICD-10 diagnoses. There’s also another model, RX-HCC, for risk adjustment of the Medicare Part D population, and there are approximately 4,200 diagnoses for this model. The CMS-HCCs predict spending for the subsequent calendar year model. The HHS-HCCs are relevant for the commercial payer population. Another model, HHS-HCCs, predicts the sum of medical and drug spending, includes all ages and predicts spending for the current calendar year.
Clinical Documentation Example
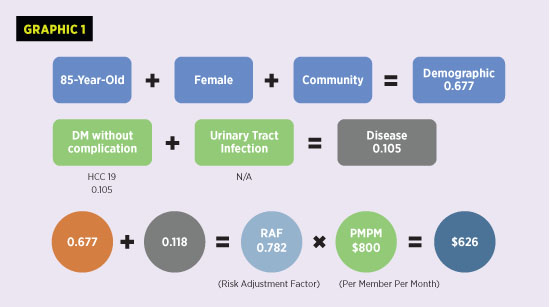
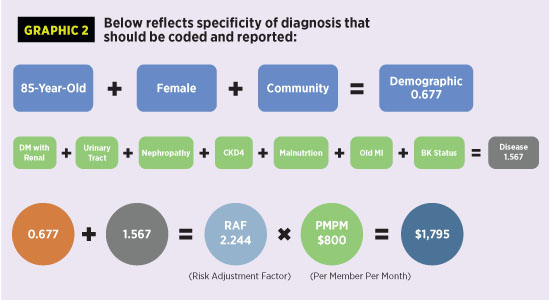
Following is an example of CMS-HCCs selected through ICD-10 coding based on clinical documentation to determine the RAF score. The comparison between the two graphics illustrates the impact of coding to the highest level of specificity.
An 85-year-old female with symptoms of painful urination, lethargy, poor appetite, dry itchy skin, and myocardial infarction one year ago. Patient is frail with recent unintentional weight loss of 30 lbs in the past six months. Patient has mild malnutrition. Urinalysis noted white blood cells, leukocyte esterase, and microalbuminuria. Serum creatinine is 1.4.
Past Medical History: Diabetes mellitus, chronic kidney disease exacerbated by diabetes, right below-knee amputation, history of myocardial infarction, baseline central retinal thickness 1.3. Lab findings revealed chronic kidney disease stage 4.
Plan: Glucophage 500 mg bid for diabetes mellitus, Cipro 500 mg orally daily for urinary tract infection, Ensure supplements for malnutrition. Return to clinic in three months. Referral to nephrologist for chronic kidney disease 4.
Graphic 1 demonstrates the lack of specificity in what is usually coded and reported to health plans in such a scenario.
Graphic 2 indicates the same scenario with the increased specificity and demonstrates what should be coded and reported.
Issues Affecting Accurate Reporting
The majority of patients are only seen in physician office settings. The office notes are limited, and specificity is not always identified. The physicians report what is evaluated, monitored, or treated and are often unaware of which diagnoses fall into an HCC category symptom. And unspecified diagnoses are not considered HCCs.
Remember, it’s important to capture all Uniform Hospital Discharge Data Set reportable secondary diagnoses, clarify diagnoses on problem lists, and review orders, home medications, and diagnostics for diagnoses not documented by providers and diagnoses that require additional specificity. Educate providers on specificity needed for complete and accurate documentation.
The following are secondary diagnoses that are sometimes not coded:
• secondary cancers;
• diabetic manifestations;
• morbid obesity/body mass index >40;
• drug dependence;
• hemiplegia due to stroke;
• monoplegia or paralysis due to stroke;
• status amputations;
• status ostomy; and
• mental disorders.
The following are few common CMS-HCCs:
• alcohol and drug dependence;
• Alzheimer’s and Parkinson’s diseases;
• angina and coronary artery disease;
• atrial fib and flutter;
• autoimmune and connective tissue diseases;
• cardiac arrest;
• cardiomyopathy;
• congestive heart failure;
• chronic kidney disease (stage 3 or higher);
• COPD
• diabetes (higher HCC score with associated manifestations);
• ileus;
• lupus;
• major psychiatric conditions;
• neuropathy (except unspecified);
• ostomy status;
• pressure ulcers stage 3, 4, and unstageable;
• seizures;
• thrombocytopenia;
• trach status; and
• vent dependence;
What’s the Bottom Line?
The RAF score represents the patient population, and the score is used to determine financial benchmarks for value-based programs.
Remember, an RAF score below 1.0 represents healthy patients, and an RAF score higher than 1.0 represent sicker patients.
HCCs represent the chronic conditions that make up the patients’ complexity, and greater specificity of the documentation can have an impact on the RAF score and subsequent reimbursement.
Whether you work in inpatient, outpatient, clinical documentation improvement, coding, or an informatics team, capturing the complete patient story is key for accurate documentation and reimbursement.
— Teresa Brown, RN, CCDS, CDIP, CCS, is a clinical analyst at 3M Health Information Systems.



