E-News Exclusive |
The Prebill Review: An Important Step for Revenue Recovery
By Mary McNerney
Health care organizations continue to face financial challenges during COVID-19. With decreased revenue, increased costs, and lower operating margins, savvy leaders need to look for innovative ways to ensure revenue integrity and financial sustainability. One proven method is a proactive approach via a prebill review—a review of documentation and coding within 24 hours of discharge and prior to the final bill (to avoid impact on discharged, not final billed). Organizations that invest in this approach ensure physician documentation supports coding compliance, Medicare severity diagnosis-related group (MS-DRG) accuracy, and quality performance data prior to claims submission. Ultimately, a prebill review promotes revenue recovery prior to claims submission.
While this is not new to many organizations, there are integral elements that define a successful framework and distinguish a prebill audit from a prebill review inclusive of a comprehensive clinical documentation improvement (CDI) program.
Prebill Audit vs Prebill Program
Is there a difference? Absolutely! A best practice prebill program incorporates an “assess, build, and sustain” approach designed to unite and align the review with data insights including impact on case mix index, education, and process improvement. Woven with physician intervention, these insights ensure optimization of revenue opportunities and risk mitigation.
This is accomplished in the following ways:
- Assess: Pinpoint opportunities through data analysis, chart reviews, and alignment of CDI to immediately recognize the greatest impact.
- Build: Design a customized program to drive education and formalization of a process to support evidence-based clinical knowledge, evoke engagement, and promote behavior change.
- Sustain: Transfer knowledge and performance measurement to ensure program sustainability. Frequent analysis using a data-driven approach is critical to program stability.
Where to Start
Perform an initial assessment to determine complication or comorbidity/major complication or comorbidity capture rates for all MS-DRGs, particularly high-frequency or high-impact DRGs, to identify your greatest areas of vulnerability and high risk. This initial look should include a review of all MS-DRGs and all payers over a brief period (eg, 30 to 90 days) to uncover missed documentation, and coding and query opportunities. It should also identify clinical documentation specialist/coder educational needs as well as physician documentation issues. Common discoveries in an initial assessment include the following:
- incorrect diagnosis and procedure code assignment;
- overlooked opportunities for application of coding guidelines;
- nonspecific physician documentation where conditions are suggested by clinical indicators
- compliance risks, including code assignment and conditions documented that lack clinical validity; and
- errors in coding complications of medical or surgical care.
Key Components of a Prebill Review Program
Once the initial assessment is completed and areas of opportunity are identified, daily prebill reviews should be implemented. These include a customized MS-DRG focus list to target opportunity for revenue capture and compliance risk. Extensive performance tracking for each MS-DRG ensures attention is directed to the areas with the greatest opportunity.
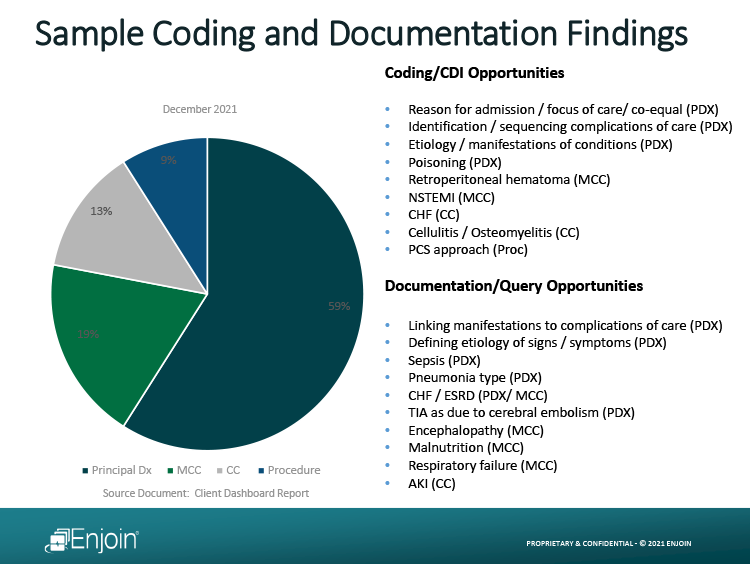
A key element of prebill reviews requires a successful balance of applying coding accuracy and clinical acumen. Ideally, the team providing these reviews possesses advanced clinical acumen and clinical coding expertise to accurately perform the reviews and provide recommendations that integrate evidence-based clinical medicine and coding rules and guidelines. According to Emmel Golden, MD, FCCP, CCDS, chief clinical officer for Enjoin, “When we conduct reviews, most of our findings are related to sequencing of principal diagnosis [See table 1]. The combination of this expertise ensures that the correct principal diagnosis is selected. Correct MS-DRG selection is key to revenue recovery and protection.”
Physicians, CDI, and coding teams each play an integral role in documentation and coding accuracy. Team collaboration with common goals is imperative to support a prebill program and the organization’s education strategy. Also, analytics gleaned from chart reviews, trend analyses, and key performance indicators should be utilized to drive customized and consistent education that supports knowledge transfer and data-driven decision making.
Other critical components include the following:
- implementation of dashboards/scorecards for transparent, actionable, and timely data for all stakeholders;
- physician education that is clinically relevant and based on his/her specific chart review findings; and
- strong operational infrastructure to support an efficient and effective process for reconciling recommendations, addressing subsequent denials, and performing ongoing monitoring.
Summary
Increasing pressures on physicians, CDI, and coding teams to deliver a return on investment and ensure “clean claims out the door” cost hospitals time and money, and can be an administrative burden. Taking a proactive, physician-led comprehensive approach will result in clinical integrity, revenue lift, and risk mitigation. Furthermore, prebill reviews complement a CDI program, support alignment of resources with organizational strategic goals, and lay the foundation for building or enhancing an effective CDI physician advisor program.
Why Perform Prebill Reviews?
- COVID-19 requires new approaches for revenue capture. Prebill reviews provide immediate revenue lift and ensure clinical and coding accuracy prior to claim submission.
- Denials are a large contributor to revenue loss and a cost burden on an already strained health care system. A proactive approach to denials protects revenue while offsetting costs.
- One-and-done audits do not contribute to an overall CDI program strategy. A prebill program supports data-driven education and process refinement for sustainability.
— Mary McNerney is chief brand officer for Enjoin.



